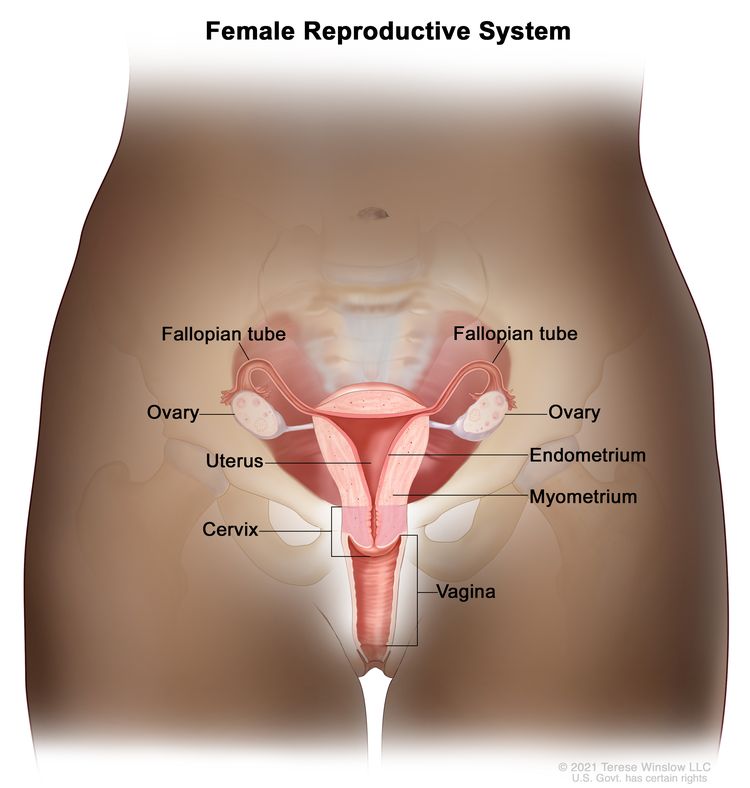
Vaginal cancer is a rare type of cancer that begins in the cells of the vagina, which is the muscular tube that connects the uterus to the external genitals. Vaginal cancer is often grouped into two main types: squamous cell carcinoma (the most common type) and adenocarcinoma. Here are key points about vaginal cancer:
Risk Factors:
- Advanced age, smoking, a history of cervical or vulvar cancer, exposure to diethylstilbestrol (DES) in utero, and certain chronic vaginal infections are associated with an increased risk.
Symptoms:
- Symptoms may include abnormal vaginal bleeding, pain during sexual intercourse, pelvic pain, and a lump or mass in the vagina.
Diagnosis:
- Diagnosis involves a pelvic examination, imaging tests (such as CT or MRI scans), biopsy, and sometimes cystoscopy or proctoscopy to assess the extent of the cancer.
Staging:
- Staging determines the extent of the cancer and influences treatment decisions.
- Stages range from I (early) to IV (advanced).
Treatment Options:
- Treatment may involve surgery, radiation therapy, and chemotherapy.
- The specific treatment plan depends on factors such as the stage of cancer and the overall health of the patient.
Survival Rates:
- Prognosis varies based on the stage of cancer at diagnosis and the effectiveness of treatment.
- Early detection and treatment contribute to better outcomes.
Prevention:
- While specific prevention strategies for vaginal cancer are limited, avoiding known risk factors, such as smoking, may reduce the risk.
Regular Checkups:
- Routine gynecological checkups are essential for early detection and monitoring of any abnormal symptoms.





